
Care Pathways
Professional descriptions of care pathways
The hospital’s care pathways are described here for professionals.
Care Pathways
23
Number of employees
725
Founded
1897
Care Pathways
Children with Epilepsy
The Neuropediatric Department has 9 care pathways for children and adolescents under 18 years old.
Continuous Spikes and Waves during slow Sleep
CSWS/ESES are characterized by changes in sleep EEG, neuropsychological symptoms, and possibly language/motor difficulties.
Children referred to a program based on CSWS/ESES are received for an initial examination by a specialist. The department plans hospitalization to monitor seizures and conduct an overnight EEG. If the patient is diagnosed with CSWS/ESES, adjustments are made to the medical treatment. A neuropsychological baseline assessment is conducted during hospitalization shortly after CSWS/ESES has ceased. Additionally, throughout the course of the illness, it is continuously assessed whether there is a need for a neuropsychological evaluation with school observation (pedagogical psychological social course).
Diagnosis and treatment
Children and adolescents from 0-17 years old who need hospitalization for further diagnosis and treatment of epilepsy are part of the ‘Diagnosis and Treatment’ program. During hospitalization, seizure monitoring with video and EEG examination is performed, and we assess whether there are psychosocial difficulties. Parents receive education about epilepsy and the management of epileptic seizures during the hospitalization.
Additionally, during hospitalization, the initiation or adjustment of medical treatment can be carried out. We also admit children with developmental disabilities (Filadelfia group 1) where examination and treatment are tailored to the child’s overall situation.
During the hospitalization, the patient is assigned a clinical specialist nurse who will maintain close contact with the patient and family going forward.
Short-term diagnosis without treatment
Assessment without treatment can take place at a specialized regional and primary care level, depending on the examination program and the severity of the epilepsy. The patient may be briefly admitted for video recording. Another option is that the patient is admitted for an EEG examination, including EMU – 24-hour video-EEG. The results are then sent to the referring physician, who will handle the ongoing treatment.
Treatment with Everolimus for Tuberous Sclerosis
It is now possible to use immunomodulatory treatment with Everolimus (Votubia) for Tuberous Sclerosis when there is also treatment-refractory epilepsy. The use of this treatment follows specifically defined criteria for patient selection and monitoring of effects and potential side effects. The treatment is managed on an outpatient basis exclusively by specialized treatment centers: Filadelfia, Rigshospitalet, and Aarhus University Hospital.
Treatment with Cannabidiol for Patients with severe epilepsy
The department offers treatment with cannabidiol to selected patients with severe forms of epilepsy, using CBD oil—the non-psychoactive component of cannabis. While there can be side effects with CBD treatment, they are rarely serious. Treatment initiation takes place during hospitalization with close monitoring of the patient regarding seizures, potential side effects, and blood tests.
Outpatient Functional Assessment of children and adolescents
The target group is children and adolescents under 18 years old with epilepsy and accompanying cognitive and/or psychosocial functional impairments who need specialized assessment of current support needs, preventive measures, and development opportunities. The program is a collaboration between the Epilepsy Hospital, Filadelfia, and the patient’s municipality of residence. The Epilepsy Hospital will handle the diagnostic and assessment part during outpatient visits. Here, we conduct a neuropsychological test to determine which areas the patient needs support and assistance with at home. After the assessment, we hold a multidisciplinary meeting across sectors to establish an action/rehabilitation plan in collaboration with the patient and their relatives. We then prepare a consensus report, which is sent to the home municipality. Referral is through the patient’s general practitioner.
Psychosocial Assessment Program
Children may be offered a psychosocial assessment program during hospitalization, lasting 2-3 weeks, upon medical referral. The purpose of the hospitalization is to evaluate the child’s cognitive, intellectual, academic, social, and psychological functional levels and provide any guidance regarding support measures and educational initiatives at home. The multidisciplinary assessment typically includes observations, tests, questionnaires, a review of available records, and interviews with the child’s parents and other relevant parties. During the admission process, a decision is made on the composition of the multidisciplinary assessment team, which may involve neuropsychologists, school consultants, educators, nurses, occupational and physical therapists, among others.
After hospitalization, a comprehensive multidisciplinary report is prepared and sent to the parents and the responsible physician, and upon agreement, to the PPR, the home school, and other relevant parties.
VNS initiation
Treatment with a vagus nerve stimulator (VNS) is offered to patients with severe epilepsy for whom neurosurgical treatment is not an option. Filadelfia has extensive experience in selecting patients for VNS treatment and performing the subsequent optimization of the stimulator. The implantation itself is performed through surgery at Rigshospitalet or Aarhus University Hospital. The initial adjustment of the stimulator is carried out during hospitalization at Filadelfia.
Epilepsy Surgery pathways
A specialist begins with an outpatient examination. Here, we plan a multidisciplinary assessment process, where a specialist and a clinical specialist nurse serve as the primary contacts.
The process includes:
- Hospitalization for seizure monitoring with 24-hour video EEG (EMU), possibly accompanied by SPECT scanning.
- Hospitalization for neuropsychological testing before surgery.
- Hospitalization after 12 and 24 months to evaluate the effectiveness of the surgery.
The assessment may include MRI scans of the brain, SPECT scans, PET scans, and MEG. Additionally, evaluations are conducted by a child psychiatrist, ophthalmologist, and physiotherapist/occupational therapist. The results of all examinations form the basis for the final recommendation for surgery in collaboration with Rigshospitalet.
Dietary treatment and monitoring
After an initial examination and blood tests, we assess which diet will be most suitable. The diet is reviewed with the family/network.
A specialist, clinical specialist nurse, and clinical dietitian provide continuous guidance and education throughout the process.
Classic Ketogenic Diet and Medium Chain Triglycerides (MCT)
The family is admitted to the department for five days, where the diet is initiated and adjusted with guidance. The admission is often accompanied by video recording of epileptic seizures and possibly additional diagnostics/treatment. Subsequent treatment is primarily outpatient with a specialist, nurse, and clinical dietitian.
Modified Atkins Diet (MAD)
The initiation of MAD is done on an outpatient basis with a clinical dietitian and clinical specialist nurse. The ongoing follow-up of the diet is managed by a specialist, clinical dietitian, and clinical specialist nurse.
Care Pathways
Adults with Epilepsy
The Neurology Department has 9 care pathways.
Diagnosis and treatment
The target group is patients from 17 years old who require prolonged hospitalization of up to three weeks for detailed diagnosis and treatment. Specially trained nursing staff conduct clinical observations. In connection with the initial outpatient examination, relevant tests are ordered: video recording of seizures, additional EEG diagnostics, including possible 24-hour hospitalization in the epilepsy monitoring unit (EMU), and possibly an MRI scan of the brain.
Diagnosis without treatment
We offer 24-hour video and EEG diagnostics during hospitalization. After discharge, we send the examination results to the referring physician.
Disabling epilepsy
Diagnosis and specialized medical treatment for patients with combined developmental disabilities and epilepsy.
The assessment and treatment include an initial outpatient examination by a specialist with specific knowledge in this area. We plan a multidisciplinary assessment process during hospitalization. Experienced staff conduct observations of the patient. We also record seizures with extended EEG, such as during a 24-hour stay in the epilepsy monitoring unit (EMU). We may refer the patient for an MRI scan of the brain, genetic testing, and other relevant examinations. Based on these results, we optimize the medical treatment. Subsequently, the patient may be referred for other treatments (surgical/VNS/diet).
Psychosocial Assessment Program
Adult patients with epilepsy who face challenges related to education, employment, or managing daily life can be offered a psychosocial assessment program during hospitalization, lasting 1-3 weeks, upon medical referral.
The medical history is supplemented with the creation of a social history, where the patient’s social situation and resources are analyzed in the context of epilepsy. The patient and their relatives are informed about strengths and weaknesses, and possible compensatory measures are identified in collaboration with the patient and their relatives.
The following examinations may be included in the program: 24-hour observation during hospitalization, neuropsychological testing, assessment of educational skills and potential for further education, fatigue level related to work functions, and evaluation of the patient’s ability to manage daily activities.
Upon discharge, we hold a network meeting where the patient, the multidisciplinary team, and all relevant municipal and other stakeholders participate as much as possible—often virtually or by phone.
We prioritize verbal communication highly. The written report follows in a comprehensive multidisciplinary document a few weeks after discharge. It is securely sent to all parties as the patient wishes.
Specialized rehabilitation for epilepsy
We admit adults aged 18 and older with epilepsy and accompanying limitations in cognitive, psychosocial, and/or physical functioning. The program lasts 6 weeks and includes observation, support, and training of the patient’s skills and ability to manage daily activities. The hospitalization is planned as two weeks inpatient + two weeks at home + two weeks inpatient. This allows the patient to try the recommended strategies at home. Upon discharge, we provide a status and assessment of the patient’s functional ability and developmental potential based on observations and examinations during hospitalization. We also assess the need for compensatory support measures at home.
We have good experience with involving relatives and municipal stakeholders in the final meeting.
As part of the cross-sectoral collaboration, we prepare a written rehabilitation plan based on the patient’s resources and needs. This plan can be sent to relevant professionals in the municipal sector with documentation to support the patient’s wishes and needs for rehabilitation at home. This is done in agreement with the patient.
PNES with or without concurrent epilepsy and psychiatric comorbidity
The treatment is aimed at diagnostically clarified patients with PNES with or without epilepsy.
It is also aimed at patients with epilepsy and psychiatric comorbidities such as stress reactions, anxiety, depression, ADHD, and autism spectrum disorders. The treatment consists of a 4-week psychotherapeutic program during hospitalization.
Referred patients are assessed for motivation and indications for a potential course of treatment. We plan the hospitalization in collaboration with the patient.
The program includes patient observation to identify stress factors and multidisciplinary cognitive milieu therapy with metacognitive interventions, such as psychoeducation, mindfulness, sensory room exercises, cognitive body therapy, self-esteem and competence training.
In collaboration with the patient, we develop a multidisciplinary cognitive problem formulation, which we use as a dynamic treatment plan.
After discharge, there is an option for a follow-up phone call with the contact person.
Dietary treatment
The purpose of the treatment is to shift the brain’s energy metabolism from being carbohydrate-based to fat-based, achieving a ketogenic state that can reduce or completely alleviate epileptic seizures.
Epilepsy patients can be referred for treatment with the Ketogenic Diet by internal neurologists or external doctors, including the patient’s general practitioner.
During the initial examination by a specialized neurologist and clinical specialist nurse, it is assessed whether the patient is a candidate for the treatment.
The patient’s resources—cognitive functions and social network—are evaluated if they are considered a candidate.
The Classic Ketogenic Diet is always initiated during hospitalization and can eventually transition to the Modified Ketogenic Diet, which is less restrictive.
The Ketogenic Diet is offered either as food the patient eats or as tube feeding.
From the start, the treatment is managed by a multidisciplinary team including a specialist doctor, clinical dietitian, nursing staff, occupational therapist, and clinical specialist nurse.
The treatment continues on an outpatient basis after the patient is discharged. The treatment typically lasts 2-3 years.
Epilepsy Surgery pathways
The process begins with an initial neurological examination. The subsequent steps involve multidisciplinary collaboration between a specialist and a clinical specialist nurse. The pathway includes multiple hospitalizations.
Hospitalization for seizure monitoring using video EEG, such as in the epilepsy monitoring unit (EMU), possibly during medication tapering.
Hospitalization for neuropsychological testing.
During the assessment process, we refer patients for an MRI scan of the brain and, if necessary, SPECT scanning, PET scanning, and MEG.
The results of all examinations form the basis for the final recommendation for surgery in collaboration with Rigshospitalet. The surgeries are performed at Rigshospitalet, while post-operative follow-ups are conducted at the Epilepsy Hospital, Filadelfia.
VNS initiation
The implantation of a vagus nerve stimulator (VNS) can be offered to patients who are not suitable candidates for epilepsy surgery. Filadelfia has extensive experience in selecting patients for VNS implantation and the subsequent optimization of the stimulator.
The implantation itself is performed at Rigshospitalet or Aarhus University Hospital, while the initial adjustment of the stimulator is usually done on an outpatient basis at Filadelfia.
In special cases, the adjustment of the stimulator may be best carried out during hospitalization.
Care Pathways
Neurophysiology Clinic
The clinic offers 7 services for children and adults.
Electroneurography (ENG General) UCGG00
Examination of the peripheral motor and sensory nerves. A neurophysiology assistant conducts the examination, and a specialist evaluates it. Indications: Carpal tunnel syndrome, nerve compression, polyneuropathy.
Electromyography (EMG/ENG) UCGG01/UCGG02
Examination of the peripheral nerves and muscles using surface and needle electrodes. If needed, we can supplement with an ultrasound examination. A specialist, and possibly a neurophysiology assistant, conducts the examination. Indication: Clinical suspicion of involvement of the peripheral nerves and/or muscles.
Visual Evoked Potentials (VEP) UCGK01
Examination of the visual pathways using light stimulation (checkerboard pattern stimulation). A neurophysiology assistant conducts the examination, and a specialist evaluates it. Indication: Multiple sclerosis.
Somatosensory Evoked Potentials (SSEP) UCGM
Examination of the peripheral and central pathways using electrical stimulation. A neurophysiology assistant conducts the examination, and a specialist evaluates it. Indication: Clinical suspicion of lesions in the central motor pathways in the spinal cord or brain.
Motor Evoked Potentials (MEP) UCGN
MEP is used to examine motor nerve pathways from the cerebral cortex through the spinal cord to the muscles. A neurophysiology assistant conducts the examination, and a specialist evaluates it.
Indication: Diseases affecting the central motor pathways from the brain to the spinal cord.
Electroencephalography (EEG)
Standard EEG ZZ141470B
EEG with Sleep ZZ1470A
Examination of the brain’s electrical activity using surface electrodes. The examination includes special provocation methods such as light stimulation and hyperventilation. A neurophysiology assistant conducts the examination, and a specialist evaluates it.
Long-term EEG Recording 1-8 Hours ZZ1470C
Used for patients with frequent seizures that are likely to occur during a few hours of recording. The brain’s electrical activity is recorded using surface electrodes along with video recording of the patient.
A neurophysiology assistant conducts the examination, and a specialist evaluates it.
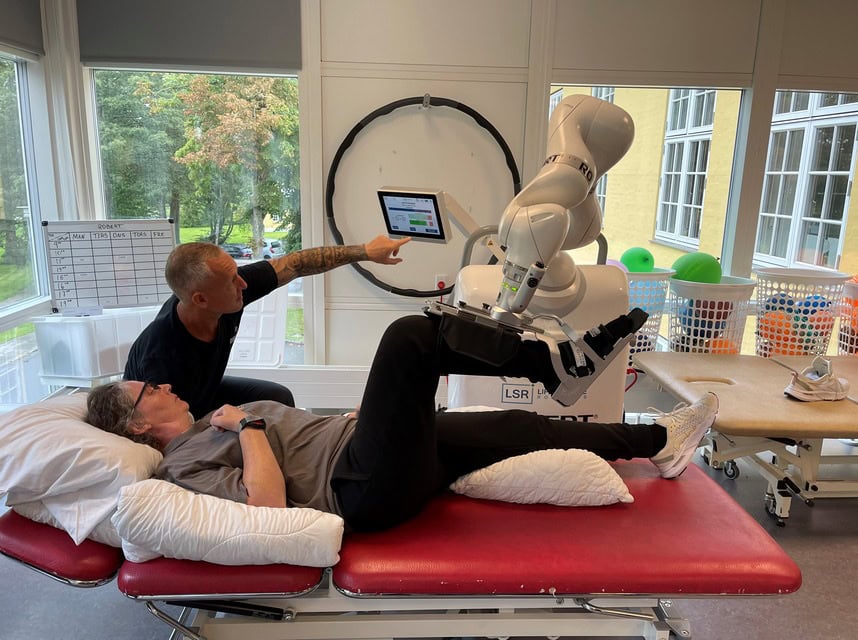
Care Pathways
Centre of
Neurorehabilitation
We begin all admissions with an intensive, multidisciplinary assessment, goal setting, and concurrent rehabilitation lasting one week. We offer rehabilitation programs at a severe or moderate level. The rehabilitation level is reassessed every four weeks. We maintain regular contact with the municipality and hold a planning meeting at the end, where the municipality receives a multidisciplinary status report.
A constant attendant is included for severe cases. If two attendants are necessary, it requires the referring authority’s acceptance of payment for one of them.

